Rachel is an Operations and Training Manager at Burlodge and a Registered Dietitian. She has conducted numerous equipment start-ups across North America. Rachel is passionate about the role food services can play in patient-centered care and helping defy the notion that hospital food can’t be nutritious and delicious.
Combating malnutrition in acute and long-term care and increasing patient satisfaction are currently two of the hottest topics in health care food services. Rightfully so. Research suggests that 45% percent of Canadian hospital patients and about 44% percent of long-
term care residents are malnourished. We also know that it’s not nutrition if it’s not eaten, and an unsatisfied patient is certainly less likely to be polishing off their plate.
How are we trying to fix this? By switching to room service, giving patients choice immediately before the meal or implementing a Spoken Menu, increasing the usage of local foods or moving towards more in-house production. These changes are undoubtedly having a positive impact.
From my experience, though, what is sometimes forgotten with these changes is the temperature of the meal by the time it reaches the bedside.
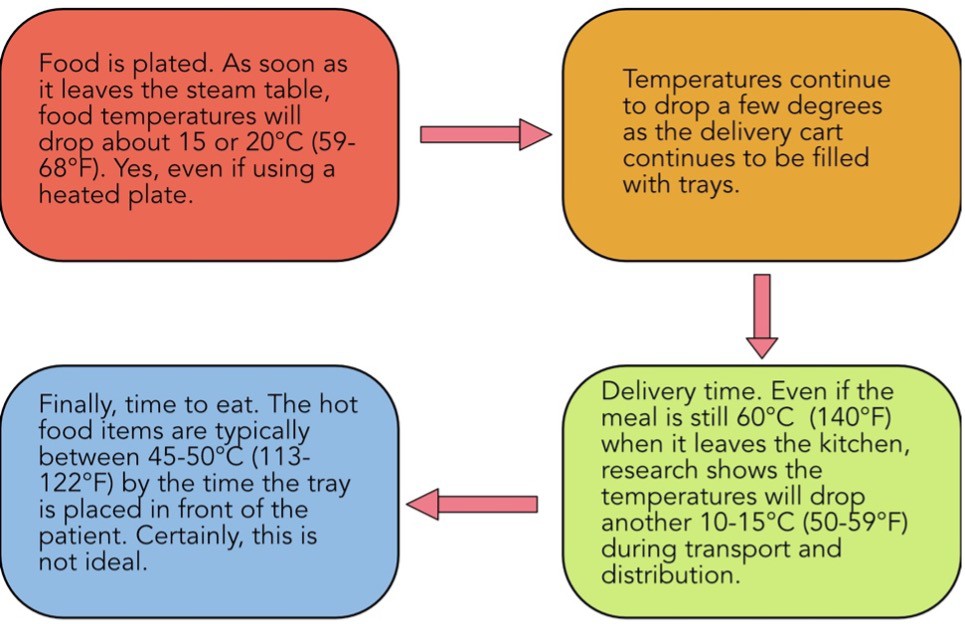
The Temperature Journey
Let’s take a look at the temperature journey of a meal when it is plated in a hot state. This assumes there is no temperature maintenance or boosting capability once a tray has been created.
While patients tell us that having choice, flexibility in mealtimes, and higher quality food are all key to satisfaction and improved intake, so is the temperature of the food itself. Research shows that:
Dissatisfaction with hot food temperatures can be a barrier to intake. The longer the patient remains in hospital, the more dissatisfied with food temperatures they become.
Hot beverages can be especially important. Few people would serve themselves a lukewarm cup of coffee at home!
Patients don’t just care about the temperature of their hot food.
Temperature of cold food and beverages is a major predicator of patient satisfaction as well.
The Benefits of Boosting
Anecdotally, I can speak to this, too. The equipment start-ups that I have found most meaningful have been those where we’ve implemented boosting equipment and made a significant impact on food temperatures at point of service. Some highlights include getting rave reviews from an elderly patient as she got to enjoy her first hot meal and cup of tea in months. We witness an incredible reduction in food waste at a long-term care home when we increased the hot food temperatures at point of service by 25 °C. In both cases there was no change to the food being served, just a change to the temperature.
Better by More than Just Degrees
When we’re eating at a restaurant, we expect our plate of pasta to be hot and our drink to be cold. Food isn’t the right temperature? We may send it back. Shouldn’t we expect the same acute and long-term care in meal service?
We can take the time to overhaul our menus, give patients choice as to what they are being served, and make mealtimes more flexible, but if the meal isn’t the right temperature, it still isn’t going to be eaten.
When assessing food waste, patient satisfaction, or considering a change to your service model, don’t forget about the impact of food temperatures, or the key role that a simple cup of hot coffee can play in brightening up a patient’s day.